My Heart is Broken - But I'm Determined
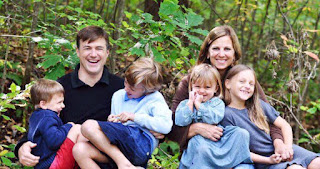
My heart is broken. Dave Bjork, Cancer Research Evangelist
has had a tough week. My friend Stephen Muir passed away yesterday. He was 45
years old, never smoked, but died of stage 4 non-small cell lung cancer. Wow.
Diagnosed August 8th, died September 4th. Wow.
I’ve been
gearing up for a major fundraising effort this fall to support the research of
Dr. Daniel Haber, the Director of the Massachusetts General Hospital Cancer
Center. The sad irony is that my friend Stephen’s story is so profoundly
relevant to the research I am supporting. I feel like there is a reason and a
purpose for my friendship with Stephen to make a difference in the work that I do
at the National Foundation for Cancer Research.
Tumors
change over time, often developing resistance to treatment. To remain
effective, targeted therapies need to address these tumor changes as they
occur. That requires constant monitoring of tumors, so that doctors can make
appropriate adjustments to patients’ treatment plans. My friend had the EGFR mutation, and there is
a targeted therapy to treat this mutation, Tarceva.
But it was too late for him. And so much work remains to get to the
point where we can diagnose cancer with a blood biopsy. This is the whole point of Dr. Haber’sresearch. We need to get to the place
where we can go for an annual physical and through a simple blood draw
determine if we have cancer. Or patients like me, can find out if our cancer
has come back.
But we need
to do the research first to get to that place where it’s really a diagnostic
blood biopsy. I’m supporting a research
project that will make a difference. Thanks to a new and exciting technology,
it is now increasingly possible to collect genetic material from tumors—even
whole tumor cells—during a routine blood draw, or a liquid biopsy. NFCR-supported
scientist Daniel Haber
and his
colleagues at Massachusetts General Hospital have developed a new technology
that allows clinicians to monitor tumor mutations as they occur, so that
treatments can be altered to address those changes in tumor biology. The
technology has the potential to radically change the way cancer is treated.
Dr. Haber
and colleagues developed a credit-card-sized device, called CTC-iChip, that can
be used to isolate minute CTCs collected via liquid biopsy and keep them viable
to analyze their drug sensitivity. Testing CTCs derived from liquid biopsies
could provide a rapid, noninvasive way to guide targeted therapy for individual
patients. If a tumor acquires resistance to a first-line treatment, this
drug-based monitoring may help to identify appropriate second-line therapy,
better enabling that one-two punch that cancer treatment can require.
In the next
phase of the research, Dr. Haber’s team will develop technology to enable
culturing CTCs collected from blood samples from patients with metastatic lung
cancer. Lung cancer is the No. 1 killer for both men and women in the United
States, causing nearly 30% of all cancer deaths each year. CTCs, which are
representative of multiple tumor lesions in patients, can be sampled repeatedly
over the course of a patient’s treatment, with minimally invasive blood draws.
The CTCs can be analyzed in the laboratory, both to watch for changes that may
occur and to evaluate the effectiveness of different drugs or drug
combinations. This step prevents the need to test drug regimens directly in
humans.
Culturing
CTCs from patients with lung cancer will likely generate a far more refined
picture of tumor composition than past technologies have produced. In addition,
focusing on genetically directed treatments will help researchers identify
potential mechanisms of disease resistance and effective drug combinations.
Results of this laboratory research would lay the groundwork for better
designed clinical trials and eventually better targeted treatments.
The
technology of liquid biopsy is poised on the cusp of truly enabling personalized
medicine – not just for patients with lung cancer, but for patients with a wide
variety of cancer types – without the need for painful, repeated biopsies. So,
in honor of my friend Stephen Muir, I persevere and support amazing scientists
like Daniel Haber.